A head injury can look minor at first, but turn serious fast. Two of the most critical traumatic brain bleeds are epidural hematomas (EDH) and subdural hematomas (SDH). They sound similar, but they behave very differently in the body and in a legal claim.
We constructed this guide to help you understand the medical differences, warning signs, and how a brain-injury lawyer builds these cases.
Emergency note: If you suspect a brain bleed, call 911 or go to the ER immediately. Worsening headache, repeated vomiting, weakness/numbness, confusion, unequal pupils, seizures, or trouble waking up are danger signs.
Quick Comparison: Epidural vs. Subdural hematoma
Feature |
Epidural hematoma (EDH) |
Subdural hematoma (SDH) |
|
Where the blood collects |
Between skull and dura |
Between dura and arachnoid |
|
Usual bleeding source |
Often arterial (classically middle meningeal artery), frequently with temporal bone fracture |
Usually bridging veins stretched/tears (falls, acceleration–deceleration) |
|
CT appearance |
Biconvex/lens-shaped, typically does not cross sutures |
Crescent-shaped, can cross sutures but is limited by dural reflections (falx/tentorium) |
|
Onset |
Often rapid (minutes–hours); classic but not universal lucid interval |
Can be acute (hours–days) or chronic (weeks–months), especially in older adults or those on blood thinners |
|
Who is at higher risk |
More common in younger patients |
More common in older adults; higher risk with anticoagulants/antiplatelets and brain atrophy |
Medical sources for the table: StatPearls (EDH/SDH), Radiopaedia review articles, Medscape imaging notes.
What Is an Epidural Hematoma?
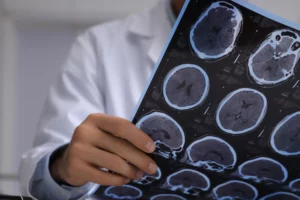
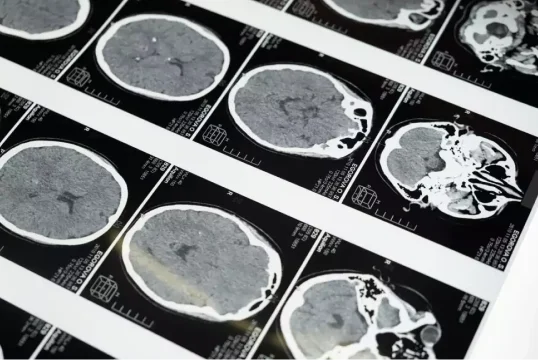
An epidural hematoma is bleeding between the skull and the dura mater, most often after blunt trauma that lacerates the middle meningeal artery (commonly with a temporal bone fracture). On a CT scan, it usually looks lens or football shaped and it stops at the skull’s seam lines (where the bones meet). EDH can worsen quickly and may require urgent neurosurgical evacuation. A “lucid interval” (brief recovery, then rapid decline) occurs in some cases.
What Is a Subdural Hematoma?
A subdural hematoma is bleeding between the dura and arachnoid, typically from torn bridging veins when the brain shifts inside the skull. On a CT scan, a subdural hematoma usually looks like a crescent. It can spread past the skull’s seam lines, but it won’t cross the brain’s inner membranes (the falx and tentorium). Acute SDH follows major trauma and can be life-threatening; chronic SDH may develop weeks after a minor hit, especially in older adults or people on bloodthinners. Treatment ranges from observation to burr-hole or craniotomy drainage, depending on size and symptoms.
Symptoms: Immediate vs. Delayed
Both EDH and SDH can present with severe headache, nausea/vomiting, confusion, weakness/numbness, seizures, or loss of consciousness. EDH tends to declare early (minutes–hours). SDH (especially chronic) can be subtle at first (worsening headaches, imbalance, memory issues) and appear days to weeks later. If any danger signs develop, seek emergency care.
Causes & Risk Factors
- Trauma: car crashes, falls, sports, assaults (EDH more often arterial after skull fracture; SDH from shearing of bridging veins).
- Age & medications: SDH risk increases with older age, brain atrophy, and anticoagulants/antiplatelets.
- Other contributors: coagulopathy and certain medical conditions can predispose to intracranial bleeding.
Diagnosis & Treatment (High Level)
Imaging
Non-contrast head CT is the frontline test; MRI can help in subacute/chronic cases
Management
Epidural: often requires urgent neurosurgical evacuation due to rapid mass effect.
Subdural: acute SDH with mass effect generally needs surgical evacuation; chronic SDH may be drained via burr holes or managed conservatively if small and stable.
Which is “More Dangerous”?
It depends on the size, location, and speed of bleeding and the patient’s overall condition. EDH can deteriorate rapidly and is a true emergency. SDH (especially in older adults) carries substantial mortality in severe cases and may be missed if symptoms are delayed or subtle. The key is fast diagnosis and the right treatment plan.
Why Hiring a Brain Injury Attorney Matters (EDH/SDH Claims)
Brain-bleed cases are medically complex and involve disputes about causation (Was the bleed from this crash or something else? Did anticoagulants make it worse? Was there a delay in diagnosis?). A focused TBI team will:
- Secure critical evidence fast: 911/CAD audio, body-cam/store video, event-data (“black box”), fall-hazard documentation, and medication history.
- Translate the medicine: Work with neurosurgeons and neuroradiologists to explain CT/MRI findings (e.g., biconvex EDH vs. crescent SDH, mass effect, midline shift).
- Prove damages the right way: Neurocognitive testing, return-to-work opinions, and life-care planning for long-term needs.
- Navigate deadlines: In California, most injury claims must be filed within 2 years (with shorter 6-month claim deadlines if a public entity is involved).
- Deal with insurers: Present a timeline that links mechanism → imaging → symptoms → treatment → losses, and push for full value.
WCTL Tip: SDH can be delayed—so if symptoms evolve after a fall or crash, return to the ER and make sure that follow-up imaging is considered.
When Hematoma vs. Hemorrhage Language Matters
A hematoma is a collection of blood (often clotted); hemorrhage refers to active bleeding. In practice, EDH/SDH may be described both ways on reports. What matters for your case is where the blood is, how much pressure it’s causing, and what treatment is required.
What to Do After a Suspected Brain Bleed
- Go to the ER (or call 911) if any red-flag symptoms appear.
- Follow medical advice and complete imaging/neurology referrals.
- Save everything: discharge summaries, CT/MRI discs, medication list, and bills.
- Call a brain-injury lawyer to protect evidence and deadlines.
Talk to an Experienced Brain-Injury Lawyer Today
If an accident led to an epidural or subdural hematoma, you don’t have to sort it out alone. We’ll move quickly to preserve evidence, coordinate with your medical team, and pursue the maximum recovery the law allows.
Call (213) 927-3700 or fill out our online contact form for a free, confidential case review with West Coast Trial Lawyers. Same-day response. You deserve the best team in California working for you non-stop.